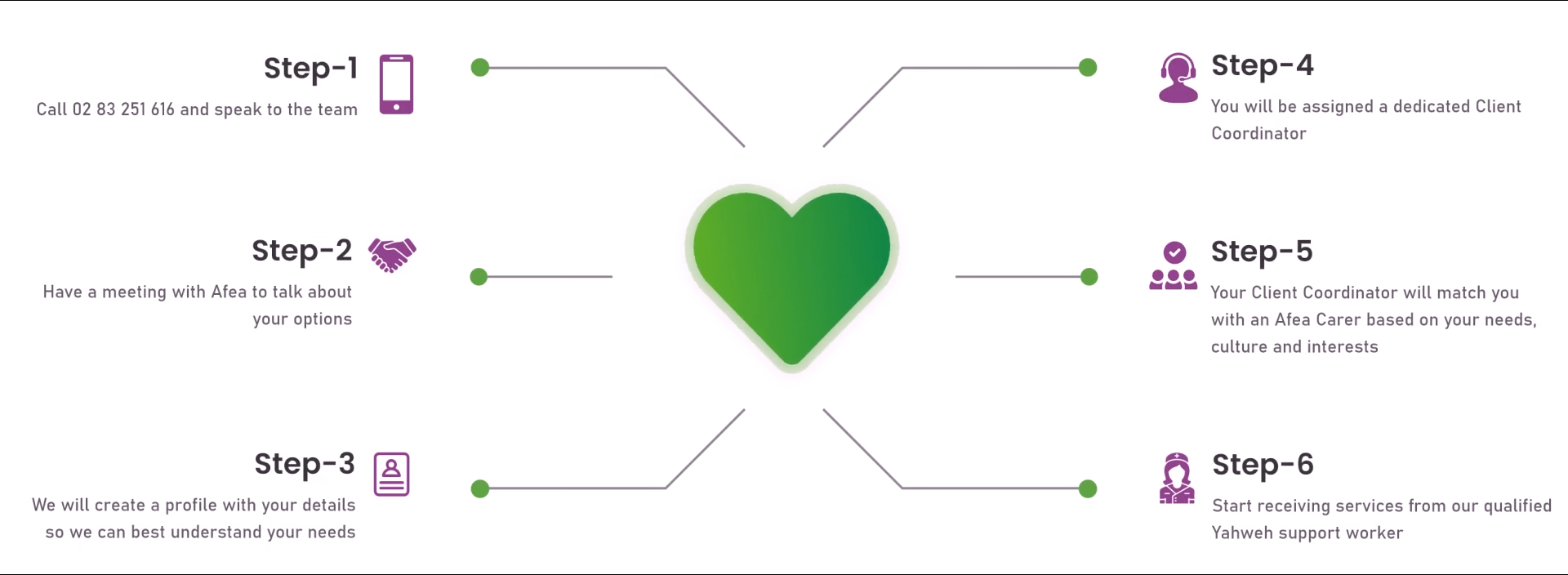
SWITCH TO YAHWEH CARE
Providing care and holistic approach to NDIS participants aiming to create opportunities for you to live your best life.
Contact UsHospital discharge summaries or reports are important. They help maintain the patient’s well-being beyond the hospital experience and provide proper treatment guidance when they continue treatment in their homes or nursing facilities. With the assistance of health professionals, the process empowers the patient with critical information concerning recovery and a follow-up visit.

Smooth hospital-to-home discharge summaries guarantee that the important patient information regarding health status, treatment, and recovery plan is transferred to the subsequent provider. This can be either a primary care physician or a home healthcare service. This reduces the likelihood of discontinuity in care, which can result in complications or mistakes.
In addition, a clear summary of the drugs prescribed upon discharge avoids medication errors once the patient returns home. This encompasses dosage, frequency, and any adjustments made during hospitalization. It also ensures the patient or caregiver knows how to use new prescriptions appropriately.
Continuity of care enables all hospital doctors and other healthcare professionals to see a patient’s history, treatment plans, and diagnoses. This reduces the likelihood of miscommunication or error, which can lead to adverse health consequences. Through the creation of long-term relationships between patients and healthcare professionals, continuity of care enables closer management of long-term conditions and early intervention.
Time spent in the hospital means more procedures, and more opportunities for complications. In other situations, readmissions also include increased opportunities for hospital-acquired infection.
When patients leave the hospital without clear knowledge of their diagnosis, care plan, or follow-up requirements, they are more likely to have complications and re-admit to the hospital. Successful recovery is possible only with proper discharge planning, such as comprehensive discharge summaries and medication instructions.
Luckily, with proper post-discharge care and instructions, the discharge summary outlines the patient’s discharge diagnosis, follow-up visits they need to attend, and symptoms that need immediate evaluation. Therefore, clear instructions reduce confusion and allow patients to take control of their recovery, ultimately reducing the likelihood of readmission.
Patients aware of their disease, treatment, and recovery process are more likely to comply with medical recommendations and adopt health-promoting lifestyles. This leads to better chronic disease management, shorter recovery time, and fewer health problems.
Empowering discharge summaries provide patients and families with vital information regarding the care of the patient’s recovery. They can include lifestyle modifications, dietary limitations, exercise, and warning signs to watch for if complications arise.
Effective education involves discussing topics specific to the patient’s condition, care plan, and individualized needs. This enables patients to adhere to their care plans and promotes better understanding between the patient/family and the healthcare team.

Jointly working healthcare discharge summaries facilitate improved communication between hospital professionals and outside healthcare providers. This collaborative work keeps everyone in the care process on the same footing. Whenever care providers actively hear about a patient’s issue, it generates confidence and compels the patient to provide essential information.
Effective communication helps patients understand their diagnosis, treatment, and course of care. Treatment compliance improves, complications are reduced, and recovery outcomes improve. This happens when patients and family members communicate effectively.
Communication needs to be tailored to the patient’s needs, e.g., level of health literacy, age, and culture. Diagrams, photographs, and written information may be especially helpful in enhancing verbal communication.
Documentation of care for future use is necessary. Electronic discharge summaries are legal health records documenting the care provided during a hospital stay. They may be used for insurance, audits, and quality control, documenting appropriate care received and helping to protect healthcare providers and patients from potential legal disputes.
Hospitals must follow rigorous regulations, such as those issued by healthcare accreditation agencies and government agencies. A discharge summary keeps healthcare institutions compliant with such regulations along with community services.
Informed consent is important. It is how a health care provider and educates a patient regarding the risks, benefits, and alternatives of a treatment or procedure provided to them so that the patient knows the options before a decision is reached. Such a notification is legally and ethically required.
Discharge summaries provide explicit direction for hospital-acquired conditions prevention following discharge by specifying clinical records such as any new diagnosis, treatment, or complications that arose during hospitalization.
Warning signs and emergency contact numbers are included in the discharge summary, making it available for patients to access information in case of an issue after discharge from the hospital. This allows for a fast and accurate response and minimizes the chances of future complications.
Most complications can be prevented with proper planning, monitoring, and communication. Note that high patient safety levels require efforts from patients, healthcare organizations, and healthcare professionals. Therefore, the process must ensure a proper understanding of treatment protocols and aim for consistent monitoring of patients during the treatment process.
Health outcomes are measurable changes in a patient’s health condition due to medical treatment. They include enhancing physical health, mental health, and quality of life after treatment or intervention.
A well-written discharge summary allows for good follow-up and support the person in obtaining follow-up on the required medical treatment, which equates to improved long-term outcomes. Whether a specialist appointment or a follow-up with physical therapy, follow-up appointments in a timely fashion can have an immense effect on outcomes.
Patient-centered care discharge summaries are also important for creating a patient-centered care experience. The patient care team will more likely accomplish the patient’s recovery goals by individualizing the discharge information to be patient-preferred and patient-specific.

Hospital discharge summaries are not administrative reports. However, they are invaluable instruments in the practice of patient care. They ensure continuity of care and reduce the risk of negative impact on mental and emotional conditions. In addition, they provide valuable information to patients and their families and improve provider communication. High-quality discharge summaries increase patient safety, reduce readmissions, and improve healthcare outcomes.
As the role of digital health tools evolves and care coordination improves, well-written discharge summaries become more vital to contemporary healthcare practices.
If you still need help following hospital discharge, contact Yahweh Care.
Providing care and holistic approach to NDIS participants aiming to create opportunities for you to live your best life.
Contact Us